Experts say the COVID-19 emergency could end this year. What would it look like?
Written by luck on January 31, 2022

(NEW YORK) — On the cusp of the third year of the COVID-19 pandemic, the United States is battling back the biggest surge of the virus yet with the omicron variant.
Cases, even while receding in some places, are near record levels. And daily deaths, while lower than the peak of last winter, are still averaging more than 2,000 nationwide.
Despite pitched battles over masks and vaccines, life appears somewhat normal in many respects — kids are going to school, people are going into work and large indoor gatherings and events are being held.
So, while it may be hard to imagine, many experts suggest 2022 could be the year COVID becomes an endemic disease, meaning it is always circulating within the population but at low rates or causing just seasonal outbreaks.
During a press conference Wednesday, Dr. Anthony Fauci, the nation’s top infectious disease expert, said the U.S. can get “sufficient control” over COVID-19 so it “does not disrupt us in society, does not dominate our lives, not prevent us [from doing] the things that we generally do under normal existence.”
This is because the virus will start running out of people to infect as people become immune and follow mitigation measures such as mask-wearing and testing if they have symptoms.
“We have the tools with vaccines, with boosts, with masks, with tests and with antivirals,” Fauci said.
As an endemic disease, COVID-19 would shift from becoming a global health emergency to a virus that the world learns to live with.
Public health experts say many societal changes are needed for a time when the virus circulates but is not as disruptive, such as targeted testing, more vaccination, better treatments and allowances for staying home when you’re sick.
“We really need to be shifting our thinking to how do we live with this virus rather than can we make it completely go away,” Dr. Timothy Brewer, a professor of epidemiology at UCLA Fielding School of Public Health, told ABC News. “So I think we need to sort of move into the mode of minimizing the impact of the virus as much as possible in terms of health, economic and social disruption — recognizing this virus is going to be there.”
People who are sick will be advised to stay home or wear masks in public
When the virus does become endemic, experts say people will be advised not go into school or work while sick and instead stay home, unlike before the pandemic.
If you have to leave the house, it could remain common to wear a mask on public transit or in indoor spaces.
“It will become a culture of if you’re sick you stay home,” Dr. Wafaa El-Sadr, a professor of epidemiology and medicine at Columbia University Mailman School of Public Health, told ABC News. “Don’t come to work, don’t go to school, don’t send your kids to school. There will be more of an appreciation of the collective responsibility that we have for each other.”
Currently, federal law does not require employers to provide paid sick leave to employees although some states, such as California, New York and Washington, have laws requiring it.
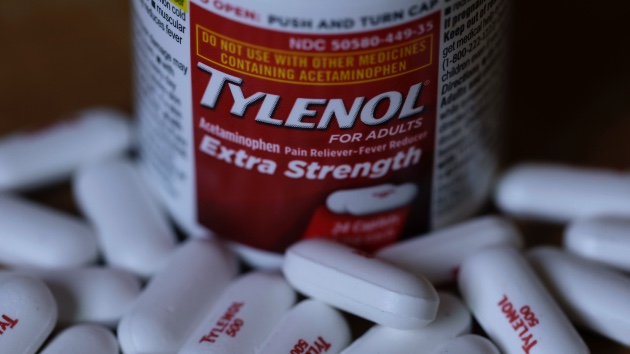
Antivirals may become more common in doctor’s offices and hospitals
In addition to vaccines, some antiviral treatments, from Pfizer and Merck, have come out in the past several months, specifically for those who test positive or had symptoms recently developed.
Studies have shown that these antivirals can help prevent hospitalization, especially those who are at high risk of severe illness.
Experts stress that even after the emergency phase is over, antivirals should not be considered a substitute for vaccines, but rather an extra layer of protection, specifically for at-risk groups.
“The distribution of antivirals is really important in terms of making sure immunocompromised people and people with disabilities have that sort of protection,” Abdulah Shihipar, a public health researcher at Brown University, told ABC News.
Brewer agrees and says he thinks the treatments for COVID-19 will be similar to those for HIV in that they will get better and better over time.
“HIV is no less pathogenic today than it was 40 years ago but the difference is we have very effective treatments, we have excellent antivirals against HIV,” he said. “So I think as antivirals become available that they will play a very important role” in combating COVID-19.
Shihipar says he hopes the federal government comes up with a long-term plan for distribution whether that means a program people can sign up for to get cheap subsidized drugs, setting up at pharmacies, delivering it to rural areas and so on.
Testing will be more strategic such as just screening people with symptoms
Currently, the U.S. has a model based on two types of testing: diagnostic for symptomatic people to see if they are positive for COVID, and preventive for asymptomatic people to make sure they are not infected before participating in activities or seeing others.
But in a world in which COVID-19 is more seasonal of a virus, experts say the country will have to shift to more focused testing, particularly focusing on the symptomatic.
“Now we kind of test just to test everybody, it should be more focused,” said El-Sadr. “For people who are symptomatic, if you have symptoms, it is a good idea to get tested, absolutely. So I think focusing on people who are asymptomatic will be very important.”
Right now, an average of 1.7 million tests is being administered per day in the U.S., according to the Centers for Disease Control and Prevention. Experts say that, during peaks, a minimum of 2 million is needed to keep up with demand. Supplies have been short in some cases as manufacturers ramp up production of at-home tests and omicron redefines infection levels in the country.
El-Sadr also says testing can be used for specific high-risk activities such as eating indoors with family members who are unvaccinated or having a social gathering with someone who is immunosuppressed as opposed to generally for indoor gatherings.
“We have to think of what is the strategic use of testing,” El-Sadr added.
Brewer believes testing programs currently in place at schools, such as students testing before returning and then undergoing weekly testing, won’t work in the long run.
“It’s logistically and financially too cumbersome and expensive and slow,” he said. “Given that we know up to 40% or more of people can be asymptomatic when infected and we know asymptomatic people can spread disease, we just kind of need to operate under the assumption that anyone is potentially infected and do things like hand hygiene and vaccination rather than relying on a testing strategy.”
Improved ventilation standards in workplaces and schools could be implemented
Experts say that improving indoor air quality will be one of the most important tasks, specifically as states begin to roll back mandates and mitigation measures.
Making sure indoor air is being recirculated will lower rates of cases and prevent outbreaks.
Shihipar says the Occupational Safety and Health Administration had standards for health care settings (which have since expired) that need to be expanded to all workplaces.
“We need to change the way we deal with indoor air, like how do we properly ventilate these spaces — not just for COVID but for flu and all these other diseases,” he said. “How do we make the air cleaner so that the disease spreads less?”
He continued, “We need emergency temporary workplace standards from OSHA. One for all workers would actually regulate employers to make their workplaces safe in terms of ventilation, in terms of capacity.”
Shihipar added that he’d like to see the government giving each teacher a certain number of portable air filters for their rooms and the governments and setting up clear standards of air regulation for school districts.
We may need annual COVID vaccines
Experts have suggested that annual COVID-19 vaccines, just like the flu shot, could become a reality in a world where the virus is endemic to keep antibody levels high.
They could even be adapted to combat variants just the flu shot is manufactured to combat which strains researchers think will be the most dominant.
Brewer said it will depend on two factors: how long immunity lasts after vaccination and how much the virus changes.
Copyright © 2022, ABC Audio. All rights reserved.